Spinal Conditions: Low Back Pain
Page Contents (click to show / hide)
Introduction
Low back pain is very common. Almost every person will suffer from an episode of back pain during his or her life. In the majority of cases it is very difficult to identify a single cause for the back pain, but, fortunately, most back pain resolves spontaneously without the need for surgical intervention.
In general, there are three types of pain: acute, recurrent acute and chronic. Acute pain is pain that starts suddenly and usually resolves in a matter of days to weeks. This accounts for over 80% of first time low back pain episodes. The source is often unidentifiable and the condition is termed simple or mechanical low back pain (see below). Chronic pain is pain that tends to last for longer than three months and this may be due to an underlying spinal condition or other factors such as muscle weakness, body weight and psychological factors / life stresses. Recurrent acute pain is pain that tends to flare from time to time.
There is a complex interaction between chronic pain and the psychological well being of a person. There is often a downward cycle of pain which, leads to the inability to perform tasks; a reliance on others; frustration and anger, anxiety and worry as to the underlying cause of the pain and what the future will hold; a lack of sleep because of pain and / or worry; and the side effects of the pain medications to name but a few. It is often difficult to break this cycle and it is understandable why people can become depressed. Most patients simply want to understand why they have back pain and what they can do to relieve it. They want an explanation. Very few patients want to undergo surgery for their pain. Unfortunately a single identifiable source causing an individual's back pain is often very hard to find and explanations can be difficult. In the majority of cases there are multiple pain sources arising from different parts of the spine that can account for the pain. This can limit the success of surgery. One of the main roles of a spinal surgeon is to exclude the serious causes of back pain and reassure the patient that they are not at risk and will not come to any harm when using his or her back. Remember, spinal surgery can be high-risk surgery that can possibly make you worse. Degenerative back pain will not kill you but on rare occasions an operation might.
False Perceptions of Spinal Problems and Low Back Pain
There are several myths and false perceptions surrounding spinal conditions. The reality is that most people at some point in their lives will suffer from back pain of some form or another, which will resolve uneventfully. For some reason the spine seems to be treated differently to other aches and pains in the body. There is a false historical belief that you must halt all activity, keep still, lie down, stay off work and stop exercise etc. There is a worry that a person will “end up in a wheelchair”, “become permanently disabled” or “be paralyzed” if they keep on using a back that is sore. It is true that in the initial phases continued activity may well make the pain appear worse. But, in the long run, avoidance of a normal lifestyle will cause more harm than good due to the reduced muscle strength and stiffness. Therefore, it is initially important to mobilise your spine and perform simple exercises at the earliest opportunity. The psychology of health beliefs plays a large role in spine related problems and it is often difficult to convince patients with simple low back or neck pain that they are not doing any harm to themselves. Only in rare cases such as trauma, tumour and infection does surgery become one of the first line treatment options. In the majority of cases surgery is the last option for back pain and only used after all other treatment modalities have been exhausted. Surgery is then only performed in very specific cases and after thorough investigation where the outcome benefits can predictably outweigh the risks of the surgery itself.
The Red Flags of Serious Spinal Pathology
Red flags are clues in someone’s story which make doctors more concerned that there may be something more serious occurring. They include the following:
- The patient is under the age of 16 or over the age of 50 with NEW onset pain
- The patient is unwell or has unexplained weight loss (not on a diet) or unexplained fevers
- The patient has a past history of cancer, recent serious illness, recent significant infection, previous long standing steroid use, HIV / AIDS, end stage renal disease, osteoporosis, Paget’s disease, alcohol or drug abuse
- The patient has widespread neurological deficits e.g. weakness in the limbs, bladder or bowel dysfunction
- The pain is non-mechanical (occurs without movement)
- The pain is in the thoracic region of the spine
- There is a deformity of the spine
- There is a history of significant trauma / injury
- The patient fails to improve with treatment
Causes of Low Back Pain
As I have previously mentioned, there are many different causes of low back pain. The commonest cause of low back pain is often referred to as simple or mechanical low back pain. This is diagnosed in the absence of any other identifiable cause. It is often of short duration and comes on after certain activities usually in the younger adult population. For example, back pain following gardening in a normally fit and well 30 year old person. The pain often comes on the following morning and is typically at the junction of the lumbar spine and sacrum. The back will feel stiff and will loosen up as the day goes on and the pain will be made worse with bending and twisting. The pain usually lasts a few days and then subsides and may not necessarily recur when the activity that precipitated it is repeated.
The following named conditions can cause low back pain:
Degenerative Disc Disease
As a person ages the spongy intervertebral discs between the bones also undergo the normal aging process. Water is lost from the discs and they become stiffer. Although we know that these degenerative discs can be the source of back pain for some reason not all people with degenerative discs are symptomatic or suffer from back pain. Recent evidence would suggest that the main factor leading to degenerative disc disease is genetic. By the age of 50 years 90% of MRI scans will demonstrate degenerative discs and this is why we can say that it is part of the normal aging process. In addition, other factors such as driving more than 1000 miles per week, people who are very overweight and smoking are associated with an increased incidence of degenerative disc disease.
Typically, low back pain arising from degenerative discs is made worse by sitting rather than standing and activities involving forward bending. It can be heightened by coughing, sneezing or straining. All of these events increase the pressure in the disc. Pain from a disc may give rise to protective spasm of the lower back muscles, which can worsen the symptoms. The symptoms tend to wax and wane over a very long period, often arising for no particular reason. Most people have good and bad days and the pain is rarely constant and debilitating.
 The mainstay of treatment for degenerative disc disease is non-operative. Physiotherapy programs, medications, core trunk stability exercises, pilates, yoga, tai chi, aqua-aerobics, osteopathy, chiropractic treatment, acupuncture, reflexology massage and other such activities can all help to improve and reduce the pain. Patients may experience low-grade continuous but tolerable pain that will occasionally flare. The frequency and intensity of the flares can be managed with an exercise programme. Due to inactivity and lack of use, the spinal muscles can become deconditioned (unfit). Their main purpose is to help you stand upright. Long periods of rest and stooping forward to relieve back pain may act to worsen the situation. When you then come to use these muscles and stand upright they are not used to the work, fatigue rapidly and start to ache. Relieved only by rest and leaning forward the vicious cycle may then continue with increasingly shorter periods of pain free use. Hence the phrase “use it or lose it”. When reconditioning your back muscles the pain may seem to get worse before it gets better. This does not mean you are doing yourself any harm. You will be using deconditioned weaker muscles that need time to re-strengthen and relearn their function in order to improve the pain
The mainstay of treatment for degenerative disc disease is non-operative. Physiotherapy programs, medications, core trunk stability exercises, pilates, yoga, tai chi, aqua-aerobics, osteopathy, chiropractic treatment, acupuncture, reflexology massage and other such activities can all help to improve and reduce the pain. Patients may experience low-grade continuous but tolerable pain that will occasionally flare. The frequency and intensity of the flares can be managed with an exercise programme. Due to inactivity and lack of use, the spinal muscles can become deconditioned (unfit). Their main purpose is to help you stand upright. Long periods of rest and stooping forward to relieve back pain may act to worsen the situation. When you then come to use these muscles and stand upright they are not used to the work, fatigue rapidly and start to ache. Relieved only by rest and leaning forward the vicious cycle may then continue with increasingly shorter periods of pain free use. Hence the phrase “use it or lose it”. When reconditioning your back muscles the pain may seem to get worse before it gets better. This does not mean you are doing yourself any harm. You will be using deconditioned weaker muscles that need time to re-strengthen and relearn their function in order to improve the pain
Only once all other treatment modalities have failed should surgery be considered. The outcomes of back pain surgery for degenerative disc disease are unpredictable. Surgery is not a cure and patients do not generally return to the way they were before the back pain started. Surgery aims to improve the symptoms by making them more manageable and to improve quality of life. As a rule of thumb, surgery for single level (only one disc is affected) degenerative disc disease has a 70% chance of working and at best gives a 70% improvement. For two level disc disease this drops to 50%. Only very occasionally is surgery performed for 3 level degenerative disc disease. The gold standard is a fusion procedure but newer techniques such as non-fusion stabilization and total disc replacements can be performed in specific cases where appropriate.
Facet Joint Degeneration
The facet joints are synovial joints. These are joints that have specialised lubricating fluid. They can develop osteoarthritis like the joints of the hip and knee. The commonest cause for facet joint degeneration is degenerative disc disease. As the intervertebral disc degenerates it can lose height and more load is then transmitted through the facet joints. This results in accelerated wear.
Facet joint pain is typically made worse by activities that stress the joints such as bending backwards, standing, reaching upwards or walking down stairs or hills. Bending forwards and “taking the pressure” off the joints such as sitting and leaning forwards typically improves it.
Facet joint degeneration and arthritis tends to occur at multiple levels of the spine. Unlike hip and knee replacements, which are very effective for treating the pain and stiffness of osteoarthritis in these joints, surgery for facet joint pain is rarely effective. Treatment of this condition usually involves non-operative measures such as medications, physiotherapy programs, core trunk stability exercises, Pilates, yoga, tai chi, aqua-aerobics, osteopathy, chiropractic treatment, acupuncture, reflexology, massage and other such activities.
Radiologically guided injections of small quantities of local anaesthetic and steroids into the facet joint can be used and can be highly effective in the short term but the pain often returns. During the pain free period following facet joint injections it is important to start exercising the spine to strengthen the muscles to help share the load going across the joints and therefore reduce the pain by protecting the joints.
Spondylosis
This term simply refers to pain caused by degenerative (often age related) changes in the spine (usually a combination of both degenerative disc and facet joint disease). It is therefore treated as discussed above for degenerative disc disease and facet joint degeneration.
Spondylolysis
A spondylolysis is a defect in the pars interarticularis part of the spine. It is present in around 5% of the population and is often asymptomatic. It is most commonly thought to be due to a growth and development problem during childhood and adolescence, although there can be other causes. It is frequently associated with activities that involve hyperextension of the spine (bending backwards) such as high diving, trampolining, gymnastics, fast bowling, wrestling and weight lifting. It can lead to low back pain of a similar nature to facet joint pain.
 With degeneration of the spongy intervertebral disc, a forward slippage of one vertebra on the other can occur (spondylolytic spondylolisthesis – see below). This can result in nerve irritation and leg symptoms as well as back pain.
With degeneration of the spongy intervertebral disc, a forward slippage of one vertebra on the other can occur (spondylolytic spondylolisthesis – see below). This can result in nerve irritation and leg symptoms as well as back pain.
The mainstay of treatment for spondyloysis is non-surgical, as described above, and with avoidance of activities that precipitate the pain. Injections of local anaesthetic and steroid into the defect can be performed to confirm the source of the pain and also to help treat it by reducing any inflammatory component. Failing this, surgery can be performed in younger patients to repair the defect. In older patients surgery is often in the form of a fusion procedure.
This topic is discussed further in the stenosis and spondylolisthesis section.
Disc Herniation
A herniated intervertebral disc, commonly known as a “disc prolapse” or “slipped disc” can result in low back pain. Discs that herniate are degenerate in nature and the low back pain is generally managed as described above for degenerative disc disease. When a disc herniates it can press on a nerve causing leg symptoms (pain, numbness and weakness). When this occurs surgical treatment is found to be more successful and reliable but only in relieving the pressure from the nerve and therefore improving the leg symptoms. The back pain may not improve with surgery.
Very rarely a disc can herniate and compress all of the nerves in the spinal canal. This can result in a condition known as cauda equina syndrome. By definition there will be involvement of the nerves to the bladder and bowel (incontinence, numbness of the genitals and buttocks). This is a surgical emergency and requires urgent intervention to prevent permanent loss in bladder and bowel function.
This topic is discussed further in the sciatica section.
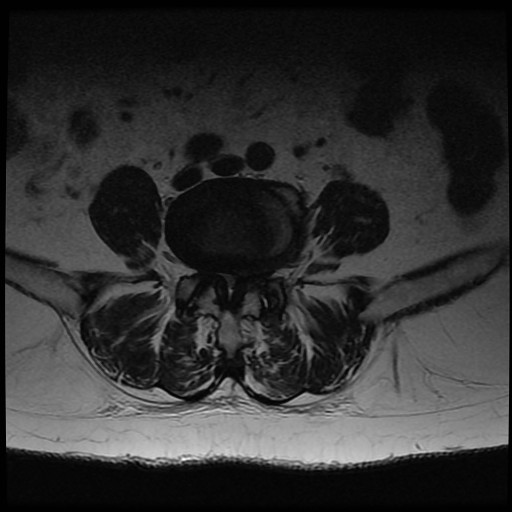
Spinal Stenosis
Spinal stenosis is a condition in which there is narrowing of the spinal canal and therefore a reduction in space for the nerves. It is usually due to degenerative changes. The intervertebral disc can be thought of as a car tyre - over time it deflates and bulges. As this occurs the height is lost at the front of the spine and the facet joints at the back of the spine start to take more load. Facet joint degeneration then occurs and the joints and ligaments can enlarge. The ligaments at the back of the spine tend to buckle inward as the disc height is reduced and they become lax. Narrowing of the spinal canal and space for the nerves then occurs due to a combination of the disc bulge, facet enlargement (hypertrophy) and ligament buckling (ligamentum flavum hypertrophy).
Spinal stenosis typically gives leg symptoms due to nerve compression. The back pain symptoms are generally due to the degenerative changes that have taken place and their management is discussed above. Occasionally when decompressive surgery is performed for leg symptoms in patients with spinal stenosis the back pain can improve but this is unpredictable. Surgery for back pain alone in spinal stenosis is rarely performed.
This topic is discussed further in the stenosis and spondylolisthesis section.
Spondylolisthesis
Not infrequently the degenerative process described above, in the spinal stenosis section, can result in a spondylolistheis. This is when one vertebra slips forward on the other. This is called a degenerative spondylolisthesis. The spinal canal can become markedly narrowed and nerve symptoms in legs can occur from compression in the narrowed spinal canal and narrowed neural foramens (the place where the nerves exit the spine). Spondylolisthesis can also occur when there is a spondylolysis and subsequent disc degeneration (a spondylolytic spondylolisthesis). There are also many other causes of a spondylolisthesis.
The treatment of spondylolisthesis depends on the cause and on the patients’ symptoms. In general, operations to relieve nerve symptoms due to nerve compression in the form of decompression are very successful. However, as a vertebra has slipped forward, removal of bone to decompress the nerves can result in further forward movement and this can lead to more problems. It is for this reason that surgeons tend to fuse that segment of the spine at the time of decompression, thereby preventing this from occurring.
Fusion procedures for spondylolisthesis can improve low back pain. This is more predictable than a fusion procedure for degenerative disc disease. It is however less predictable than a decompression procedure for compressive nerve symptoms in the legs. The reason for this is that the vertebrae have moved into an abnormal position and may be moving in an abnormal fashion. Stopping the abnormal movement is thought to reduce the back pain.
This topic is discussed further in the stenosis and spondylolisthesis section.
Spondylitis
Spondylitis means inflammation of the spine. Typically this occurs in conditions such as rheumatoid arthritis and ankylosing spondylitis. A small amount of inflammation will occur with the degenerative change discussed above.
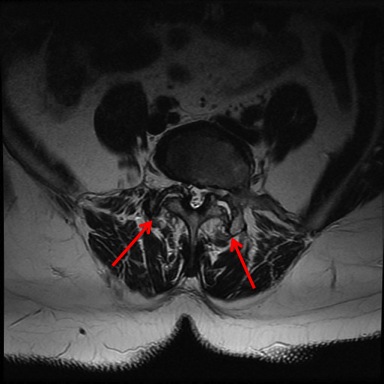
Sacroiliac Joint Pain
The sacroiliac joints are found between the sacrum and the pelvis at the lower end of the spine. The ligaments surrounding these joints are the strongest in the body. Sacroiliac joint pain is very difficult to diagnose and can be even more difficult to treat. It can be a cause of buttock, low back and posterior thigh pain. Physical examination can be very challenging in identifying the pain source and no radiological imaging studies consistently provide findings that are helpful in diagnosing sacroiliac joint pain. Pelvic belts and physiotherapy may help relieve the pain. Local anaesthetic and steroid injections can be difficult to perform given the complex anatomy of the joints and may need to be executed under CT guidance. They can be both therapeutic and diagnostic. Surgery for sacroiliac joint pain should only be undertaken after all other causes of the pain have been excluded. Only a surgeon who regularly carries out the procedure should perform it.
Spinal Deformity (Scoliosis and Kyphosis)
Scoliosis is defined as a curvature of the spine beyond that of normal when viewed from the front. Kyphosis is defined as a curvature of the spine beyond that of normal when viewed from the side. Spinal deformities can cause back pain. The pain may be due to the underlying cause of the deformity or the altered position of the spine and subsequent effect on normal function. In very simplistic terms if you were to lean to the side or forwards all day then you will probably develop low back pain. Treatment is aimed at the underlying cause.
Spinal Trauma, Infections and Tumours
Injuries to the spine, infections and tumours can all cause back pain. It is important that these are excluded as a cause of back pain as they are all serious conditions. Doctors use the “red flags” described above to help them determine whether the pain is due to a serious underlying condition. Once the diagnosis has been confirmed with radiological imaging the treatment will then depend on the underlying cause, the patients’ medical fitness and both the patient and families wishes.
Pathology from Elsewhere
Low back pain can arise from other areas not just the spine. Abdominal conditions affecting the aorta, pancreas, kidneys, stomach and bowel can all cause back pain. Likewise gynaecological conditions of the ovaries and uterus can also cause low back pain. Treatment is then targeted at the underlying condition.
Pregnancy Related Back Pain
There are two common types of low back pain during pregnancy. The first is typical low back pain. This is due to any underlying conditions discussed above, the weight gain during pregnancy, the shift in the bodies’ centre of gravity and the hormone surges associated with pregnancy. About 50% of women will have back pain during pregnancy. The mainstay of treatment is conservative with physiotherapy and good posture control. It normally settles after the pregnancy but may continue if an underlying condition has been rendered symptomatic.
The second cause is pelvic pain due to hormone induced ligamentous laxity. The normally rigid bony pelvic ring becomes more lax in order to permit the passage of the baby through the birth canal. A pelvic brace and physiotherapy may help to control the symptoms. Fortunately the ligaments usually stiffen up again in the 6 weeks following birth and the pain subsides.
There are also other causes for low back pain in pregnancy such as the position of the baby and underlying obstetric problems.
The Yellow Flags of Low Back Pain
As mentioned above, there is a complex interaction between chronic pain and the psychological well being of a person. We term the factors that increase the risk of developing, or perpetuating long-term disability and work loss associated with low back pain ‘Yellow Flags’. Identification of risk factors should lead to appropriate intervention. Red flags should lead to appropriate medical intervention; yellow flags to appropriate cognitive and behavioural management, which are also vitally important in the treatment of low back pain. The main aim is to help the person experience less distress and disability.
Examples of yellow flags include:
- The belief that pain is harmful or disabling
- The belief that all pain must be abolished before attempting to return to work or normal activity
- The expectation of increased pain with activity or work
- Fear of increased pain with activity or work
- Constantly thinking the worst about your back
- The avoidance of normal activities
- Reporting extremely high intensity of pain e.g. above 10 on a 0 to 10 scale
- High intake of alcohol or other substances (possibly as self-medication)
- Lack of financial incentive to return to work
- The experience of conflicting diagnoses or explanations for back pain resulting in confusion
- Lack of satisfaction with previous treatment for back pain
- Depression
- Feeling under stress and unable to maintain sense of control
- Feeling useless and not needed
- Lack of family support
- Unsupportive or unhappy current work environment
Coming to Terms with the Underlying Cause of Chronic Low Back Pain
It is often difficult for patients to come to terms with the fact that they have a condition that causes them pain and for which there is no easy solution or quick fix. It is important to communicate these feelings with healthcare professionals, family and friends. Developing psychological coping strategies and positive management plans to help deal with the pain and the underlying condition are important.
Further Information on Low Back Pain
More information about low back pain can be found in the following documents and in the Useful Links section of this website. Please note that some of these documents are written for health care professionals.
I have several exercise videos reproduced on this website.
KnowYourBack.org is the website of the North American Spine Society and contains a lot of useful information.
The “How to Beat Pain” programme from the BBC is an excellent video:
Dr Mike Evans has an introductory video for low back pain:
Mr P. Sell, Consultant Spinal Surgeon, explains back pain in this video:
Advice on how to quit smoking:
Advice on obesity form patient.co.uk
Advice on how to improve your fitness
Back Pain Basics from the North American Spine Society
BackCare exercises for back pain
National Institute of Clinical Excellence (NICE) Low Back Pain Guidelines
NHS England National Low Back and Radicular Pain Pathway
Non Specific Low Back Pain in Adults from patient.co.uk
Information on depression from the NHS
Information on depression from patient.co.uk